Modifier 25 is used to indicate that on the day a procedure was performed, the patient’s condition required a significant, separately identifiable E/M service above and beyond what was included with the procedure that was provided.
Full Reimbursement Policy document from Cigna: click here
Pertinent Minor Procedure Codes click here
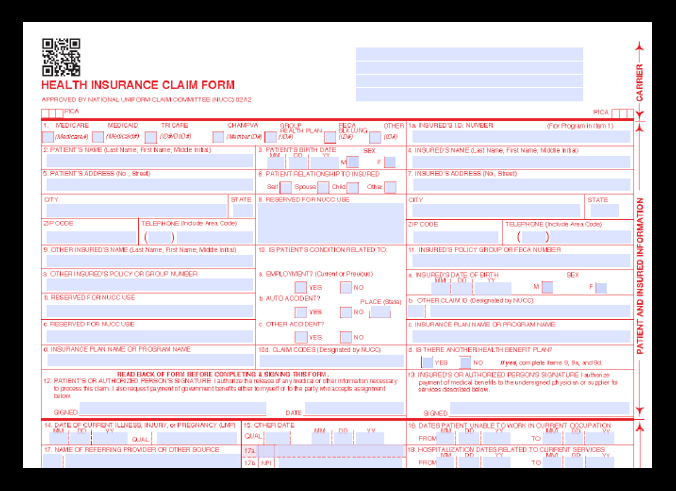
CLAIMS SUBMISSION DETAILS:
Claims should continue to be submitted electronically to Cigna, even if supporting documentation is required.
Indicate in the PWK (Claim Supplemental Information) segment of Loop 2300 of the electronic claim that the documentation will be sent through another channel. The indicators on the electronic claim includes the delivery method (PWK02) for sending the attachment (e.g., fax, mail), as well as the description code (PWK01) for the type of attachment (e.g., physician report, operative notes).
The attachment indicators or a text reference to an attachment should not be placed in the NTE (Claim Note) segment of Loop 2300 of the electronic claim. Cigna will not recognize that attachments were sent if the indicator or other attachment reference is sent in the NTE segment of Loop 2300 of the electronic claim. The provider must work with their electronic data interchange (EDI) vendor to be sure the appropriate fields on the electronic claim are completed.
When submitting the attachments, please list the member name, member ID and/or policy number per the Cigna Reference Guide to each page.
Supporting documentation must be faxed to CIGNA at 1.833.462.1360.