Providers are increasingly responsible for quality, cost and outcomes in their populations of patients.
MetroCare is committed to providing the tools and resources to help member physicians succeed in the value-based environment.
The following information is provided for educational purposes only and should not be regarded as clinical or legal advice. Metrocare, Inc. does not ensure the accuracy of this information and does not guarantee that following this information will result in receiving any government payment. It is the attesting healthcare providers responsibility to comply with all program requirements.
Practice Management Support
Credentialed members of MetroCare have access to provide health plan coverage and extended benefits services for themselves and their staff. click here SVMIC provides so many services free of charge to their policyholders and practice staff. SVMIC Services page click here UNITEDHEALTHCARE NEWS and LINKS UHC Monthly Network Updates click here UHC Surest Plan: Click here for Surest Information Web Page Surest Scoring: Click here UHC Healthcare Professional Online Training: CLICK HERE UHC MA Referral Process: VIDEO HERE CIGNA NEWS and LINKS Cigna Provider Newsroom: network updates/policies/tools/resources/digital services click here Cigna Healthcare Professional Online Training: CLICK HERE HealthChoice Health Plan HUB Services
SVMIC Services
Cigna and UHC Payer Information
click here for slide deck
Medicare Initiatives
Advanced Primary Care Management Services
APCM services combine elements of several existing care management and communication technology-based services you may have already been billing for your patients.CLICK HERE FOR DETAILS
Opioid Use Disorder Screening & Behavioral Health
Medicare pays for opioid use disorder (OUD) screenings performed by physicians and non-physician practitioners. If you diagnose your patient with OUD, they also pay for treatment services. CLICK HERE FOR DETAILS
CLICK HERE for CMS letter to physicians regarding behavioral health services for your patients.
Telehealth Services
Telehealth services have been expanded during the COVID PHE (public health emergency). Because of relaxed billing and coding rules during the PHE, the Office of the Inspector General will soon be auditing telehealth claims for proper coding/billing/payment. CMS has provided some helpful resources to assist practices with billing compliance. CLICK HERE FOR CMS WEBPAGE WITH LATEST GUIDES ON TELEHEALTH.
The Center for Connected Health Policy has a series of videos titled " Telehealth 101" that can be very helpful CLICK HERE TO ACCESS
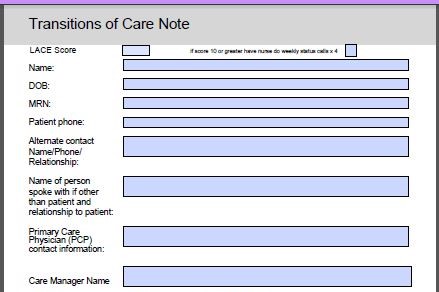
Transitional Care Management (TCM)
Transitional Care Management is the coordination and continuity of care for a patient being discharged from a specific facility type back into their community. To prevent a gap in their care, the provider accepts responsibility for care of the patient with moderate or high complexity medical problems immediately upon discharge.
The following documents, a detailed MLN summary(front and back) from CMS, and practice templates for workflow, are presented for your reference:
Update 2025 (click image above). TCM Assessment Tool, Workflow, and Template (click image).
Wellness Visits (IPPE/AWV)
Medicare wellness visits are yearly appointments to assess and update the condition of your Medicare patients for the purpose of creating and implementing a preventive health plan tailored to each specific patient with patient counseling and education to support that plan.
These encounters are not routine visits for physical examination and treatment of conditions. They can, however, be performed in conjunction with a routine visit to avoid scheduling a separate appointment to address conditions requiring attention. Access CMS Module here
IPPE (G0402)
Initial Preventive Physical Examination (Welcome to Medicare visit)
Focus on health promotion and disease prevention and detection
ACCESS IPPE TOOLKIT (click)
Initial AWV (G0438) and Subsequent AWV (G0439)
Initial Annual Wellness Visit (first AWV- one-time only):
Creation of a preventive health plan for the coming 5-10 years using risk assessment, screens, etc.
Subsequent AWV:
Yearly update to initial assessments, conditions, and screening schedule with education, counseling, and referrals
MACRA / MIPS
The following information is provided for educational purposes only and should not be regarded as clinical or legal advice. Metrocare, Inc. does not ensure the accuracy of this information and does not guarantee that following this information will result in receiving any government payment. It is the attesting healthcare providers responsibility to comply with all program requirements.
MACRA / MIPS OVERVIEW
This value-based payment format for Medicare was enacted as part of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. It allowed for the Medicare SGR (sustainable growth rate) to be abolished.
Measurement began in 2017 with Reporting in 2018 and (fee schedule) Adjustment in 2019.
MIPS, the Medicare Incentive Payment System, combines three previously existing Medicare quality programs: PQRS, Meaningful Use, and Value Modifier.
Some providers are exempt form the MIPS program but may opt in.
Check your MIPS reporting eligibility by entering your NPI on this page: https://qpp.cms.gov/participation-lookup
MIPS - Medicare Incentive Payment System
https://qpp.cms.gov/mips/overview
MIPS is a four-part program that involves practice reporting in three areas:
1. Quality Measures- formerly PQRS https://qpp.cms.gov/mips/quality-requirements
2. Promoting Interoperability- formerly Meaningful Use https://qpp.cms.gov/mips/promoting-interoperability
3. Practice Improvement Activities-value based activities often associated with Patient Centered Medical Home designation. https://qpp.cms.gov/mips/improvement-activities
4. Cost, gathered from your Medicare claims and formerly a part of the Value Modifier, is not reported separately by you and now counts more than ever.
https://qpp.cms.gov/mips/cost
The cost portion of MIPS will be impacted by the level of risk coding submitted by your practice on your Medicare claims. We offer frequent coding webinars for physicians and staff on our activity calendar.
Your Plan
1. Continue to update your strategic plan yearly, as MIPS reporting requirements increase along with possible negative payment adjustment increases.
2. Use your EHR better. Use an EHR. Become more proficient in using your EHR. Claims reporting is not sufficient for MIPS reporting any more.
3. Make sure your EHR software is current. The PI requirements specify a current version. Contact your vendor to update your software, if necessary.
4. Get help. Good performance in MIPS to avoid a negative fee schedule adjustment requires higher scoring and has been increasing in difficulty each year. Specialty providers should consult their professional associations which often have excellent advice and registries to assist their specific practice types. Your software vendor may assist with direct reporting from your EHR.
5. Participate in a Medicare Shared Savings Program or other APM option. CMS is encouraging this option for everyone.
MetroCare Trilogy CIN Network Initiatives
Preventive Visits for Commercial Plans
Preventive Health
Preventive Campaigns
In October 2016, MetroCare instituted a targeted plan toward establishing population health efforts in our practices by bringing data and source materials for breast cancer, cervical cancer, colorectal cancer and STD screenings.
MetroCare quality reporting coordinators meet with our practices and upload trend reports via Citrix Sharefile that further define opportunities to improve care along with controlling cost.
We are working with our practices to more firmly establish these steps to further develop their practice plan toward value-based care. Links below are comprehensive information our commercial contract payer coverage in 2024.
MetroCare Publications
Delivering Value
Delivering Value February 2026 Edition
Delivering Value December 2025 Edition
Delivering Value October 2025 Edition
Delivering Value August 2025 Edition
Delivering Value June 2025 Edition
Delivering Value April 2025 Edition
Delivering Value February 2025 Edition
Delivering Value December 2024 Edition
Delivering Value October 2024 Edition
Delivering Value August 2024 Edition
Trilogy Lo Loestrin Fe Pharmacy Newsletter
Delivering Value June 2024 Edition
Delivering Value April 2024 Edition
Delivering Value 2024 New Year Edition
Delivering Value 2023 Wrap/ Annual Meeting Edition
Delivering Value October 2023
Delivering Value Special Spring Edition 2023
Trilogy Poly-Pharmacy Newsletter:SSRIs
Delivering Value February 2023
Delivering Value 2022 Annual Meeting Edition
Delivering Value October 2022
Trilogy Poly-Pharmacy Newsletter: PPIs Sept 2022
Delivering Value February 2022
Delivering Value December 2021